Bone Health & Osteonecrosis After COVID‑19: Causes, Diagnostics, Treatment & Prevention
Causes & Risk Factors
-
Corticosteroid use
In severe COVID‑19 with respiratory distress, corticosteroids like dexamethasone or methylprednisolone are often used. These can impair blood flow to bone tissue, leading to cell death (osteonecrosis). -
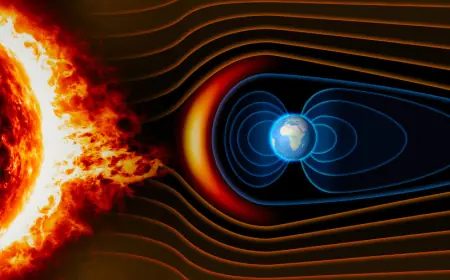
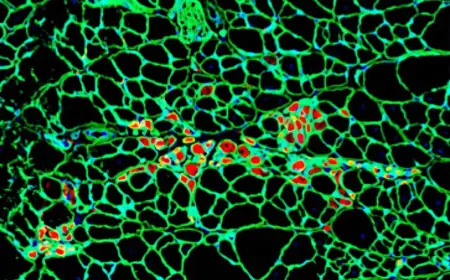
Vascular and thrombotic issues
Micro‑emboli, small clots, and disturbed blood flow during or after COVID‑19 can reduce oxygen/nutrient supply to bone and contribute to osteonecrosis. -
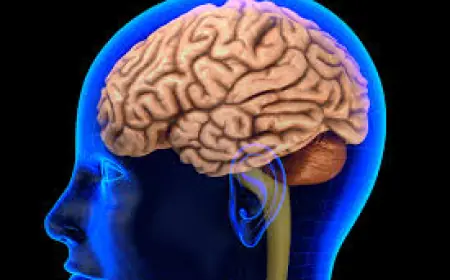
Inflammatory responses and immune dysregulation
High inflammation, elevated cytokines, strong immune responses, and disease severity all increase risk of damaging bone microstructure. -
Dose and duration
Higher doses, longer steroid courses, earlier onset of symptoms, and more severe illness raise the risk.
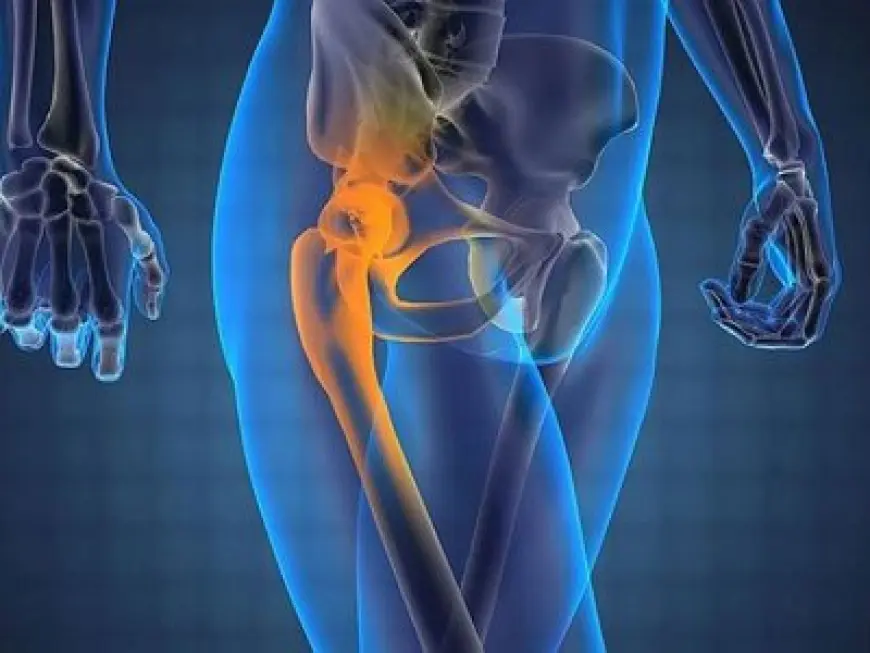
Diagnostics
-
Clinical assessment & symptoms
Pain, especially in hip area; limping; movement restriction; worsening with activity. -
Screening
For people in risk groups (e.g. those who used steroids), periodic evaluation; MRT is the most reliable for early detection. -
Radiological classification
Systems like Ficat, ARCO to define stage, presence of collapse, degree of necrosis.
Treatment
| Stage | Treatment Approach |
|---|---|
| Early (Ficat I–II, no collapse) | Conservative management: rest, avoid weight‑bearing, NSAIDs, Vitamin D & bone support agents; follow‑up MRT. |
| Intermediate (Ficat II‑III, beginning collapse) | Core decompression; PRP / BMAC therapies; physical therapy & rehabilitation. |
| Late (Ficat IV, structural collapse, loss of joint function) | Total joint replacement (prosthesis); bone grafting; long recovery and rehab period. |
Prevention
-
Use corticosteroids only when necessary, at minimal effective dose, shortest duration possible.
-
Maintain adequate Vitamin D & calcium levels; good nutrition.
-
Regular safe physical activity.
-
Periodic imaging (MRT or X‑ray) for those at risk.